Obesity and mortality: challenging the conventional wisdom, part III: BMI is nearly useless
by Alan Cohen
I’ve just written a couple posts critiquing the recent study in the Journal of the American Medical Association claiming that overweight people are at lower risk of mortality. This is the third and last, and will be a detailed exploration of why BMI is a bad metric of obesity.
I am certainly not the first to claim this, and indeed there are many researchers who have been defending measures such as waist circumfrence for years. But my point is not just to trash BMI, nor to defend another measure in particular (I think waist circumfrence is also a red herring), but rather to use BMI as an example of how shoddy thinking can lead to the adoption of poor metrics and thus serious public health consequences.
Problem #1: optimal BMI depends on the individual
My BMI is around 24, toward the higher end of “normal.” For me, this is a relatively healthy weight. My friends John and BriAnne responded to my first post by indicating that they are at 25.8 and 19.5 respectively, making them “overweight” and “normal” according to standard guidelines, and they are also at healthy weights. Neither John nor I has a very robust or muscular body type; there are many men who will certainly have much higher BMIs than either of us, and will be at nearly perfect weights for their physiques. BriAnne is quite slender; a man with her height-to-weight ratio might be unhealthy. So clearly the best BMI depends on body type, gender, genetic background and many other factors. And it changes with age. I showed in my last post how BMI does not apply in the elderly.
Problem #2: BMI doesn’t measure what we think it does
In addition to changing in old age, optimal BMI is quite different in children:
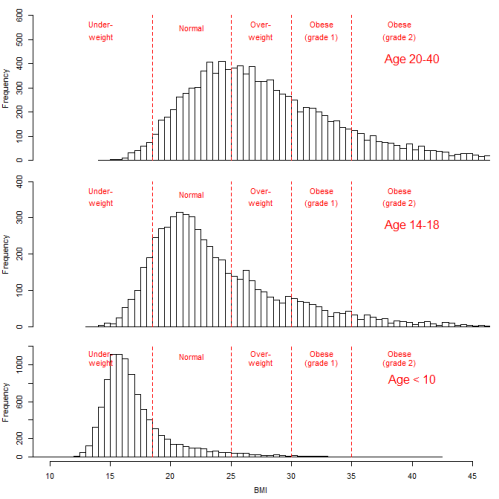 Again, this is public data from NHANES in the US. Most children under 10 are “underweight” according to the standard cut-offs. In one sense, this doesn’t matter, because the pattern is so clear that pediatricians are surely aware of it, and are not counseling children with a BMI of 15 to put on a few more pounds. But it is still important because it shows how the height-weight relationship changes with age, in surprising ways.
Again, this is public data from NHANES in the US. Most children under 10 are “underweight” according to the standard cut-offs. In one sense, this doesn’t matter, because the pattern is so clear that pediatricians are surely aware of it, and are not counseling children with a BMI of 15 to put on a few more pounds. But it is still important because it shows how the height-weight relationship changes with age, in surprising ways.
I’ve always thought of toddlers as a bit chubby. They have big heads relative to their body size. I would have expected toddlers to have a high BMI; instead, they have BMIs so low they would be considered unhealthy in adults. I’m not sure why this is (though I’m sure someone knows); one guess is that body composition (fat, muscle, etc.) is very different in children. Another guess is detailed below. Whatever the case, it means that the relationship of height to weight as represented by BMI is not a general indicator of obesity, and should cause us to question what it means in adults.
Problem # 3: individual versus population risk
As Mathieu Roy pointed out to me recently, BMI may be a better measure of population risk than of individual risk. That is, if you know the BMIs of all the adults in your population, you may be able to predict heart disease or diabetes rates pretty well. This is not the same thing as being able to say what the risk is for any given patient based on her BMI.
The reason for this is the individual differences outlined in Problem #1. Some individuals at BMI 25 will be at relatively high risk because, based on their body type, they should be at 20 or 21 – those extra 4 points make a substantial difference. Other individuals are at their ideal weight at 25. For example, I am 6 feet (184 cm) tall, 177 lbs (80 kg), BMI 24. If my ideal weight based on my body type were 20, that would mean I was overweight by 30 lbs (14 kg). Conversely, now I could weigh in at BMI 20 and be officially considered normal, yet be substantially underweight.
If individual differences in optimal weight were small relative to the BMI scale, this would not be a problem. For example, if the ideal BMI was between 21 and 22 for everyone, BMI might work relatively well as a measure of obesity. But because there is so much individual variation, BMI is essentially uninterpretable as a measure of individual risk – there is just too much noise and not enough signal.
This will all average out at the population level, as long as the population has the same percentage composition of body types and risk profiles as the one used to establish the BMI cutoffs. That is, two populations that differ only in their BMI distributions but not in sex ratio, age distribution, ethnic composition, and genetic factors, will likely have differ in their risk profiles for chronic diseases in ways that are relatively predictable based on BMI. This does not mean we should use BMI as a population measure, for reasons I address below.
Problem #4: BMI is too simplistic
BMI is weight/height². This formula is simple and easy to calculate. It gives us a measure that incorporates the relationship between height and weight, taking into account that weight will not change linearly with height because height is a one-dimensional measure, whereas weight is largely a function of volume, which is three dimensional.
However, this is unlikely to be the correct formula. For example, if we compare metabolic rate and body size across mammal species, we find that metabolic rate is proportional to mass to the two-thirds power. This is an approximation – the true power cannot be estimated precisely, but may be around 0.62. Many relationships in nature are like this – they don’t work out to nice round numbers like 2 just because we want them to and it’s convenient to calculate. If we wanted to tweak the formula, height should almost certainly be to a power other than two (and probably larger, given that volume is three dimensional and that my BMI, as a tall person, is overestimated by the current formula).
So why is height squared in BMI? Probably because it was convenient and not too far off. But “not too far off” doesn’t cut it in this case. If the power of height is “not too far off” but just a little too small, it will mean that we are systematically overestimating the BMI of tall people and underestimating the BMI of short people. It is probably for this reason that children have such low BMIs.
This kind of systematic error causes all kinds of problems. For example, BMIs in Japan will appear to be healthier than those in the Netherlands, even if there is no difference in terms of having height-appropriate weights. A generational change in early childhood nutrition that causes people to grow taller can appear to be a generational epidemic of obesity. And a tall patient can be counseled to lose weight when he shouldn’t, whereas a short patient might not be counseled to lose weight when he should.
It would be possible to identify the most appropriate power for height empirically with an algorithm to find the power that minimizes the differences in BMI distributions across people of different heights. (This method might pose a few problems, but would be a substantial improvement over current estimates.)
Where does this leave us?
Many of the problems with BMI are known to experts, who generally suggest using alternative measures such as waist circumfrence. But this knowledge has not stopped one of the world’s most prestigious medical journals from accepting a paper based solely on the use of BMI, and has not stopped the conclusions from being heavily publicized in the media. It is hard to say for sure, but it is not unlikely that all the conclusions of this article would have changed had they had access to more accuate measures.
So what is to be done? I can’t single-handedly convince the medical establishment to abandon BMI. Perhaps I will get around to developing an improved index, though I think that will only solve a few of the problems. The best solution would be to have an algorithm that could predict an individual’s ideal weight (based on age, sex, height, genetic background, race, percent body fat, and so forth) and to always use some measure of the actual weight relative to ideal weight.
But even this would continue to put too much emphasis on weight and not enough on eating well. As I’ve said before, I think both weight problems and health problems are side effects of eating poorly; I think the direct effects of weight on health are relatively minimal, except in those people who have metabolic disorders or who have already eaten very poorly for a very long time and thus achieved a relatively extreme weight.
I look forward to reading your comments!
I think you have missed the point of the paper you are trying to criticize, which is to show what happens when you use the standard categories.. You might just as well say that the paper itself supports your point that there may be something wrong with the categories because the “normal weight” category has higher mortality than the “overweight” category. So what you don’t like is calling those categories by those names.
Also by the way those are categories for adults only so there is no point in comparing them to children.
Hmmm, I don’t pretend to know what Flegal and colleagues were thinking, but the last sentence of the abstract is “The use of predefined standard BMI groupings can facilitate between-study comparisons.” This seems to me a fairly ringing endorsement for standardized BMI categories independent of contextual factors such as age. I am not just opposed to the names we give the categories, but to the idea of categories per se in cases like this.
However, I agree with you that it is widely known that BMI categories apply to adults, not children. The point I was trying to make was that the particular way they don’t function in children supports the hypothesis that BMI, as currently calculated, is biased low for short people and biased high for tall people.
[…] hard-nosed reasons to be wary of trying to measure things that are not easily measurable – risks of bias, misaligned incentives, and missing important information that is harder to quantify. But, as a […]